Bone and suture anchors
Contents
- 1 Overview
- 2 Bone, suture, and tissue anchors
- 2.1 Materials of sutures
- 2.2 Types
- 2.3 Mechanism
- 2.4 Ideal suture characteristics
- 2.5 Essential suture characteristics
- 2.6 Other suture characteristics
- 2.7 Possible failure mechanisms
- 2.8 Suturing techniques
- 2.9 Suture anchoring methods
- 2.10 Other information on suture
- 2.11 Conditions treated by bone, suture, and tissue anchors
- 2.12 Treatment methods and procedures
- 2.13 Advantages and disadvantages of various treatment procedures
- 2.14 Other facts
- 3 Market data for conditions and various treatment procedures
- 4 Overview information on the patents in these areas
- 5 Competitors in these areas
Overview
The complete or partial detachment of ligaments, tendons and/or other soft tissues from their associated bones within the body are relatively commonplace injuries, particularly among athletes. Such injuries are generally the result of excessive stresses being placed on these tissues. By way of example, tissue detachment may occur as the result of an accident such as a fall, over-exertion during a work-related activity, during the course of an athletic event, or in any one of many other situations and/or activities.
In the case of a partial detachment, the injury will frequently heal itself, if given sufficient time and if care is taken not to expose the injury to further undue stress. In the case of complete detachment, however, surgery may be needed to re-attach the soft tissue to its associated bone or bones.
Numerous devices are currently available to re-attach soft tissue to bone. Examples of such currently-available devices include screws, staples, suture anchors and tacks. source
History and Development
History
The history of sutures begins more than 2,000 years ago with the first records of eyed needles. The Indian plastic surgeon, Susruta (AD c380-c450), described suture material made from flax, hemp, and hair. At that time, the jaws of the black ant were used as surgical clips in bowel surgery. In 30 AD, the Roman Celsus again described the use of sutures and clips, and Galen further described the use of silk and catgut in 150 AD. Before the end of the first millennium, Avicenna described monofilament with his use of pig bristles in infected wounds. Surgical and suture technique evolved in the late 1800s with the development of sterilization procedures. Finally, modern methods created uniformly sized sutures.
Catgut and silk are natural materials that were the mainstay of suturing products, and they remain in use today. The first synthetics were developed in the 1950s, and further advancements have led to the creation of various forms. The different types of sutures offer different qualities in terms of handling, knot security, and strength for different purposes. No single suture offers all of the ideal characteristics that one would wish for. Often the trade-off is in tissue handling versus longevity versus healing properties.
Development
Arthroscopic techniques for stabilization of the shoulder have continued to evolve over the past decade.
- Initially staples, rivets, screw-washer combinations and plates were developed for securing soft tissues.
- Numerous complications were experienced with these devices, such as:-
- Migration,
- Breakage,
- Irritation/infection,
- Need for removal and/or anatomic placement limitations.
- In the worst of scenarios, significant articular surface damage and/or synovial fistulae were the result of such complications.
- Further evolutionary advances have lead to arthroscopic intra-articular suture techniques, where "hardware" devices are not needed.
- The complications are rare with suture techniques, these procedures are difficult to master and are again subject to anatomic placement limitations as well as suture cutout and/or pullout.
- Further advancement is the introduction of suture anchors.
- These devices have the potential to avoid the anatomic placement limitations, irritation and need for subsequent removal found with "hardware" fixation devices.
- In addition, because of their ability to be precisely placed where needed, the problems of cutout and/or pullout are dramatically reduced. source
Bone, suture, and tissue anchors
Bone anchors or suture anchors are devices which attach soft tissue to bone. This may be achieved by tieing one end of a suture to soft tissue and the other end to a device which "anchors" the suture to the bone. source
- Suture anchors are small, there are many variations of design approach.
- Anchors come in any number of configurations - deployable, bioresorbable, screw-in, or screw-in with a washer.
- Materials include titanium, coated titanium, or stainless steel to name a few. Moreover, it can be preloaded or stand-alone models, and from various suture sizes.
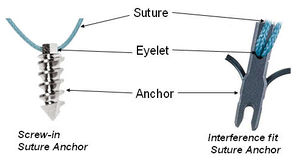
Suture Anchors are very useful fixation devices for fixing tendons and ligaments to bone. They are made up of:
- The Anchor - which is inserted into the bone. This may be a screw mechanism or an interference fit (like a rawlbolt used in DIY). They may be made of metal or biodegradable material (which dissolves inthe body over time).
- The Eyelet - is a hole or a loop in the anchor to through which the suture passes. This links the anchor to the suture.
- The Suture - is attached to the anchor by through the eyelet of the anchor. It also may be a non-absorbable material or a biodegradable material
Suture anchors are small devices placed in bone that have attached sutures or other materials that can be used for repair of soft tissues structures. They are most commonly used in the shoulder and knee regions for reattaching ligaments and tendons. There are several different designs including screws and metal posts with attached barbs. source
Materials of sutures
Choice of suture material depends on:source
- Properties of suture material
- Absorption rate
- Handling characteristics and knotting properties
- Size of suture
- Type of needle
Choosing the right suture material
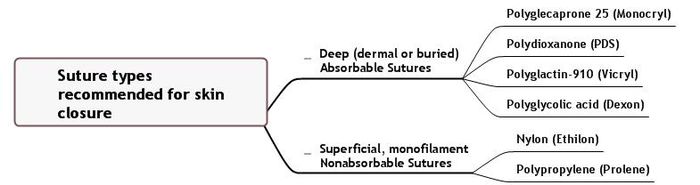
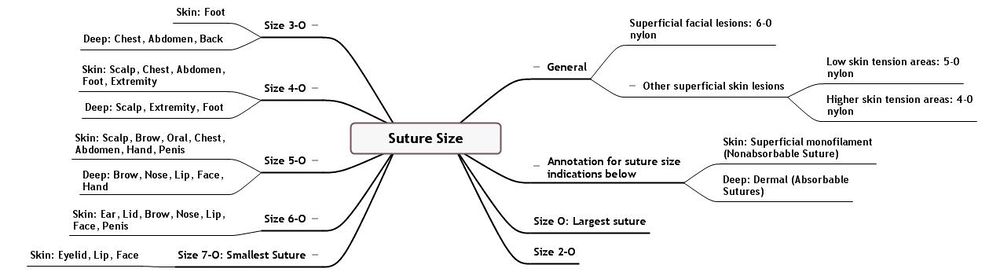
Types
- Absorbable sutures:
- Absorbable sutures are made of materials which are broken down in tissue after a given period of time, which depending on the suture can be from ten days to four weeks.
- They are used therefore in many of the inner tissues of the body.
- In most cases, three weeks is sufficient for the wound to close firmly.
- The suture is not needed any more, and the fact that it disappears is an advantage, as there is no foreign material left inside the body and no need for the patient to have the sutures removed.
- Nonabsorbable sutures:
- Nonabsorbable sutures are made of materials which are not metabolized by the body, and are used therefore either on skin wound closure, where the sutures can be removed after a few weeks, or in some inner tissues in which absorbable sutures are not adequate.
- This is the case, for example, in the heart and in blood vessels, whose rhythmic movement requires a suture which stays longer than three weeks, to give the wound enough time to close.
- Other organs, like the bladder, contain fluids which make absorbable sutures disappear in only a few days, too early for the wound to heal.
- Inflammation caused by the foreign protein in absorbable sutures can amplify scarring, so if removable sutures are less antigenic it would represent a way to reduce scarring.
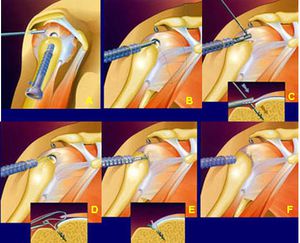
Mechanism
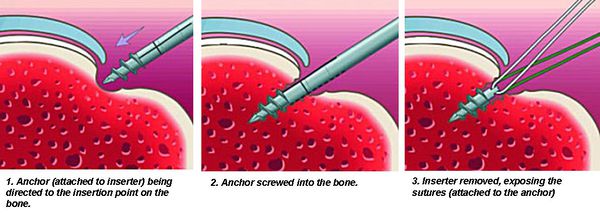
The anchor is inserted to the bone and the suture attaches to the tendon - thus fixing the tendon to the bone via the suture-anchor device {figure below)
Ideal suture characteristics
The ideal suture has the following characteristics:
- Sterile
- All-purpose (composed of material that can be used in any surgical procedure)
- Causes minimal tissue injury or tissue reaction (ie, nonelectrolytic, noncapillary, nonallergenic, noncarcinogenic)
- Easy to handle
- Holds securely when knotted (ie, no fraying or cutting)
- High tensile strength
- Favorable absorption profile
- Resistant to infection
Unfortunately, at the present time, no single material can provide all of these characteristics. In different situations and with differences in tissue composition throughout the body, the requirements for adequate wound closure require different suture characteristics.source
Essential suture characteristics
All sutures should be manufactured to assure several fundamental characteristics, as follows:
- Sterility
- Uniform diameter and size
- Pliability for ease of handling and knot security
- Uniform tensile strength by suture type and size
- Freedom from irritants or impurities that would elicit tissue reaction source
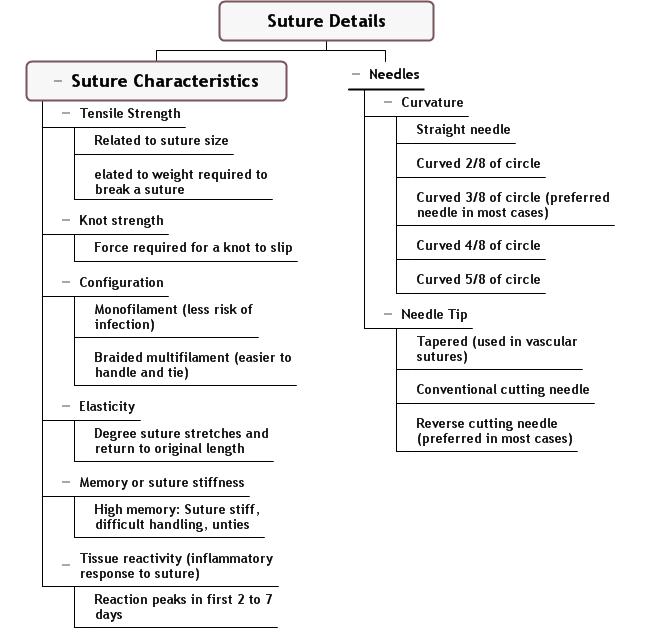
Other suture characteristics
The following terms describe various characteristics related to suture material:
- Absorbable - Progressive loss of mass and/or volume of suture material; does not correlate with initial tensile strength
- Breaking strength - Limit of tensile strength at which suture failure occurs
- Capillarity - Extent to which absorbed fluid is transferred along the suture
- Elasticity - Measure of the ability of the material to regain its original form and length after deformation
- Fluid absorption - Ability to take up fluid after immersion
- Knot-pull tensile strength - Breaking strength of knotted suture material (10-40% weaker after deformation by knot placement)
- Knot strength - Amount of force necessary to cause a knot to slip (related to the coefficient of static friction and plasticity of a given material)
- Memory - Inherent capability of suture to return to or maintain its original gross shape (related to elasticity, plasticity, and diameter)
- Plasticity - Measure of the ability to deform without breaking and to maintain a new form after relief of the deforming force
- Pliability - Ease of handling of suture material; ability to adjust knot tension and to secure knots (related to suture material, filament type, and diameter)
- Straight-pull tensile strength - Linear breaking strength of suture material
- Suture pullout value - The application of force to a loop of suture located where tissue failure occurs, which measures the strength of a particular tissue; variable depending on anatomic site and histologic composition (fat, 0.2 kg; muscle, 1.27 kg; skin, 1.82 kg; fascia, 3.77 kg)
- Tensile strength - Measure of a material or tissue's ability to resist deformation and breakage
- Wound breaking strength - Limit of tensile strength of a healing wound at which separation of the wound edges occurs source
Possible failure mechanisms
- Soft tissue strength: One possible failure mechanism is suture cutting through the soft tissue to which it is tied. This is something all suture retaining devices have in common. This failure mechanism is dependent only on the suture, soft tissue and surgical technique so the failure mechanisms involving the bone anchor may be evaluated independently of the soft tissue strength.
- Suture strength: The suture is a probable point of failure, partly because the suture is usually weaker than the anchor. The suture may fail at the anchor, knot or some unexpected flaw mechanically isolated from the anchor.
- Bone or anchor strength:The anchor may fracture and loosen from the bone or the bone may fracture, resulting in anchor displacement from the bone due to inadequate fixation. Bone fractures are more likely to occur at bony sites which contain greater amounts of cancellous or more porous bone.
- Suture fatigue resistance: Notching of the suture as the suture rubs against bone or the anchor during cyclic motion may result in suture breakage. This may not be an important issue except in special applications where healing would not be sufficient to bear expected loads by six weeks.
- Anchor fatigue resistance: Cyclic stresses in the device may exceed the endurance limit of the anchor design, resulting in device fracture, loosening and loss of fixation. This may not be an important issue if the tissue heals soon (less than six weeks). source
Suturing techniques
Simple suture or everting interrupted suture
Insert the needle at a 90° angle to the skin within 1-2 mm of the wound edge and in the superficial layer. The needle should exit through the opposite side equidistant to the wound edge and directly opposite the initial insertion. Oppose equal amounts of tissue on each side. A surgeon's knot helps place the nonabsorbable suture. Strive to evert the edges and avoid tension on the skin, while approximating the wound edges. Place all knots on the same side.
Simple running suture
This suture method entails similar technique to the simple suture without a knotted completion after each throw. Precision penetration and tissue opposition is required. The speed of this technique is its hallmark; however, it is associated with excess tension and strangulation at the suture line if too tight, which leads to compromised blood flow to the skin edges. Another variant is the simple locked running suture, which has the same advantages and similar risks. The locked variant allows for greater accuracy in skin alignment. Both styles are easy to remove. Additionally, the running sutures are more watertight.
Mattress suture
Vertical mattress sutures can aid in everting the skin edges. Employ this technique also for attachments to a fascial layer. The needle penetrates at 90° to the skin surface near the wound edge and can be placed in deeper layers, either through the dermal or subdermal layers. Exit the needle through the opposite wound edge at the same level, and then turn it to repenetrate that same edge but at a greater distance from the wound edge. The final exit is through the opposing skin edge, again at a greater distance from the wound edge than the original needle entrance site. Place the knot at the surface. A knot placed under tension risks a stitch mark.
The horizontal mattress can be used to oppose skin of different thickness. With this stitch, the entrance and exit sites for the needle are at the same distance from the wound edge. Half-buried mattress sutures are useful at corners. On one side, an intradermal component exists, in which the surface is not penetrated. Place the knot at the skin surface on the opposing edge of the wound.
Subcuticular suture
Sutures can be placed intradermally in either a simple or running fashion. Place the needle horizontally in the dermis, 1-2 mm from the wound edge. Do not pass the needle through the skin surface. The knot is buried in the simple suture, and the technique allows for minimization of tension on the wound edge. In a continuous subcuticular stitch, the suture ends can be taped to the skin surface without knotting.
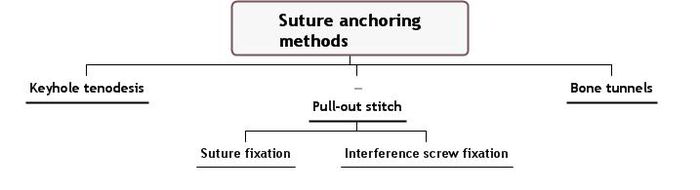
Suture anchoring methods
Keyhole tenodesis
- The "keyhole" tenodesis requires the creation of a bone tunnel in the shape of a keyhole, which allows a knotted tendon to be inserted into the upper portion, and subsequently wedged into the lower narrower portion of the tunnel where inherent traction on the tendon holds it in place.
- This technique is challenging as it is often difficult to sculpt the keyhole site and insert the tendon into the tunnel.
- In addition, if the tendon knot unravels in the postoperative period, the tendon will slide out of the keyhole, losing fixation.
Pull-out stitch
- With this technique, sutures attached to the tendon end are passed through bone tunnels and tied over a post or button on the opposite side of the joint.
- This technique has lost favor in recent years due to a host of associated complications, which include wound problems, weak fixation strength, and potential injury to adjacent structures.
Bone tunnels with either suture fixation, or interference screw fixation
- The most common method of fixation of tendon to bone is the use of bone tunnels with either suture fixation, or interference screw fixation.
- The creation of bone tunnels is relatively complicated, often requiring an extensive exposure to identify the margins of the tunnels.
- Drill holes placed at right angles are connected using small curettes. This tedious process is time-consuming and fraught with complications, which include poor tunnel placement and fracture of the overlying bone bridge. Graft isometry, which is easy to determine with single point fixation, is difficult to achieve because the tendon exits the bone from two points.
- After creation of tunnels, sutures must be passed through the tunnels to facilitate the passage of the tendon graft. Tunnels should be small enough to allow good tendon-bone contact, yet large enough to allow for graft passage without compromising the tendon.
- This portion of the procedure is often time-consuming and frustrating to a surgeon. Finally, the procedure can be compromised if the bone bridge above the tunnel breaks, resulting in loss of fixation.
- The technique restricts fixation to the strength of the sutures, and does not provide any direct tendon to bone compression.
Other information on suture
Conditions treated by bone, suture, and tissue anchors
- Avulsion fractures
- Bicipital Tendon Injuries
- Collateral Ligament Pathology, Knee
- Distal Humerus Fractures
- Knee Dislocations
- Lateral Epicondylitis
- Mannerfelt Syndrome
- Meniscal repair
- Medial Humeral Condyle Fracture
- Patellar Tendon Rupture
- Perilunate Fracture Dislocations
- Posterior Glenohumeral Instability
- Quadriceps Tendon Rupture
- Recurrent Ankle Sprains
- Stener Lesion
- Superior Labral Lesions
- Superior Labrum Lesions
- Triangular Fibrocartilage Complex Injuries
- Wrist Arthroscopy
Treatment methods and procedures
Soft tissue re-attachment procedures utilizes following ways:
Screws The detached soft tissue is typically moved back into its original position over the bone. Then the screw is screwed through the soft tissue and into the bone, with the shank and head of the screw holding the soft tissue to the bone.
Staples The detached soft tissue is typically moved back into its original position over the bone. Then the staple is driven through the soft tissue and into the bone, with the legs and bridge of the staple holding the soft tissue to the bone.
Suture anchors
- An anchor-receiving hole is generally first drilled in the bone at the desired point of tissue re-attachment. Then a suture anchor is deployed in the hole using an appropriate installation tool. This effectively locks the suture to the bone, with the free end(s) of the suture extending out of the bone. Next, the soft tissue is moved into position over the hole containing the deployed suture anchor. As this is done, the free end(s) of the suture is (are) passed through or around the soft tissue, so that the free end(s) of the suture reside(s) on the far (i.e., non-bone) side of the soft tissue. Finally, the suture is used to tie the soft tissue securely to the bone.
- The soft tissue may first be moved into position over the bone. Then, while the soft tissue lies in position against the bone, a single hole may be drilled through the soft tissue and into the bone. Next, a suture anchor is passed through the soft tissue and deployed in the bone using an appropriate installation tool. This results in the suture anchor being locked to the bone, with the free end(s) of the suture extending out of the bone and through the soft tissue. Finally, the suture is used to tie the soft tissue securely to the bone.
- In some cases, the suture anchor may include drill means at its distal end, whereby the suture anchor can be drilled into the bone, or drilled through the soft tissue and into the bone, whereby the aforementioned drilling and anchor-deployment steps are effectively combined.
Tacks The detached soft tissue is typically moved back into its original position over the bone, and then a tack-receiving hole is generally drilled through the soft tissue and into the bone. Then the tack is driven through the soft tissue and into the bone, so that the shaft and head of the tack will hold the soft tissue to the bone.
Advantages and disadvantages of various treatment procedures
Disadvantages:
- The structure of the anchor may be vulnerable to breakage due to mechanical stresses affecting the anchor during its fixation to tissue.
- Eyelet failures have been reported to originate from stresses that are caused when sutures attached to the anchor are pulled taut.
- Sutures can become twisted during the insertion of screw type anchors, hindering the completion of the repair in most conventional anchors, the suture eyelet is a small ring, or a hole that forms a pulley surface to enable suture running.
- Suture running friction due to the small radius of the pulley aspect of the eyelet, and suture damage due to sharp portions of the anchor near the suture running path.
- The pull-out strength, i.e. the force needed to pull the anchor out of the hole where it has been fixed, may be quite low.
Other facts
- Tissue adhesives: In recent years, topical cyanoacrylate adhesives ("liquid stitches") have been used in combination with, or as an alternative to, sutures in wound closure. The adhesive remains liquid until exposed to water or water-containing substances/tissue, after which it cures (polymerizes) and forms a flexible film that bonds to the underlying surface. The tissue adhesive has been shown to act as a barrier to microbial penetration as long as the adhesive film remains intact. Limitations of tissue adhesives include contraindications to use near the eyes and a mild learning curve on correct usage.
- Antimicrobial sutures: Another recent development in wound closure involves the use of sutures coated with antimicrobial substances to reduce the chances of wound infection. While long-term studies are not yet available, preliminary results indicate that these sutures are effective at keeping bacteria out of wounds.
- Polymethylmethacrylate can be used to augment anchor fixation, reducing the risk of anchor pull-out failure, regardless whether the suture anchor hole is stripped or unstripped. source
Market data for conditions and various treatment procedures
Number of patients by geography
- IN AUSTRALIA, about 12% of the population, and 34% of people over 50 years of age, suffer from osteoarthritis. The most commonly affected joint is the knee - Adam B Chapman (2003)
Number of patients by procedure
- There are approximately 400,000 rotator cuff repairs performed globally each year. This number will continue to grow due to the aging population and the increased activity level of this age group
- Rotator cuff injuries are quite common within all demographic categories due to daily wear and tear of the tendons
- The soft tissue anchor market segment is projected to have a higher than average annual growth rate with the majority of the growth coming from bioabsorbables - Source
- Although the number of arthroscopic procedures undertaken for knee osteoarthritis in Australia is not available, a considerable proportion of the 56 000 knee arthroscopies performed each year would be for knee osteoarthritis - Adam B Chapman (2003)
Projected size of patient populations
Overview information on the patents in these areas
Queries used on patent database
- Search strategy:-
- Database: MicroPat
- Key word search both in full text search and title abstract search (in INPADOC)
- Assignee search (identified by web search) List of assignee
- Search query:-
- Full text search:
- Query 1: ((Bone* OR suture*) AND anchor*) AND (ligament* OR tendon* OR tissue* OR bone*))
- Query 2: ((Bone* SAME anchor* OR suture* SAME anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (anchor* SAME suture* SAME tissue* SAME bone*))
- Query 3: ((Bone* WITH anchor* OR suture* WITH anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (anchor* WITH suture* WITH tissue* WITH bone*))
- Query 4: ((Bone* WITH anchor* OR suture* WITH anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (anchor WITH component*) AND (anchor* WITH suture* WITH tissue* WITH bone*))
- Query 5: ((Bone* WITH anchor* OR suture* WITH anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (anchor WITH component*)) US or Any IPC: A61*
- Query 6: ((Bone* WITH anchor* OR suture* WITH anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (Arthroscop* OR orthro*) AND (anchor* WITH component*)) US or Any IPC: A61*
- Query 7: ((Bone ADJ1 anchor* OR suture ADJ1 anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (Arthroscop* OR orthro*) AND (anchor ADJ1 component*)) US or Any IPC: A61*
- Query 8: (((Bone* OR suture*) WITH anchor*) AND (ligament* OR tendon* OR tissue* OR bone*) AND (Knee OR shoulder))
- INPADOC search: ((Bone* OR tissue*) AND (anchor* OR fix*5) AND suture*)
- Full text search:
- Period of search: 1836 to date
- Merged all the search results
- Removed duplicates and family patents
- Total patent counts: 3183
- Preparation of excel sheet
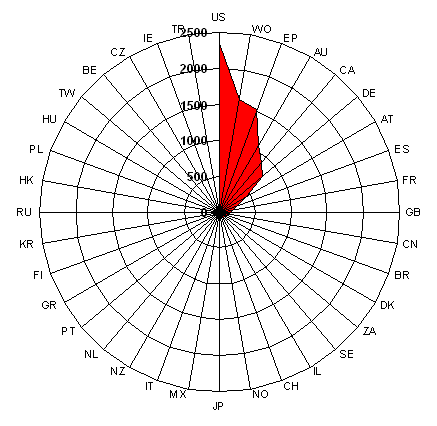
Patents by geography
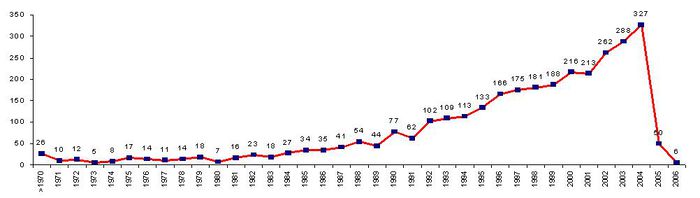
Patent timeline
The IP activity initiated during early 70s, and a continuous increase in the IP activity evident thereafter, with maximum activity during the year 2004.
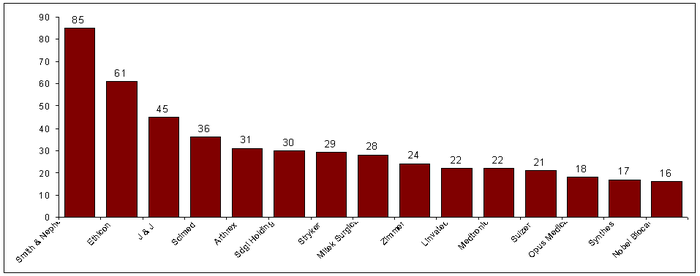
Patents by assignees
Assignees with more than 15 records are considered as major players.
- Ethicon is a part of J & J. source
Visual patent landscape snapshot
Components of anchors and features - An interactive model
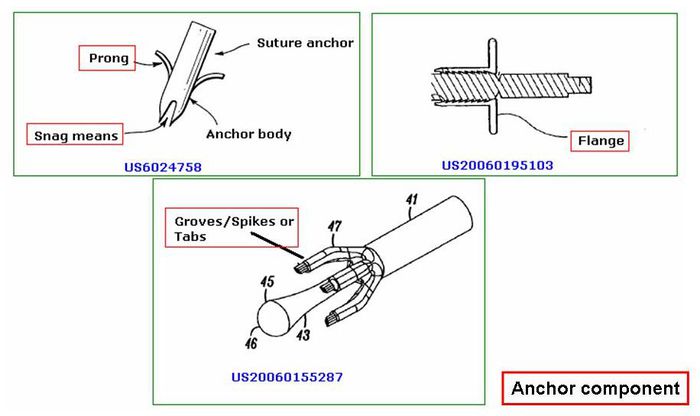
Various anchor components
- Prong - for securely holding the anchor (US6024758)
- Snag means - for engaging or grabbing a suture loop element (US6024758)
- Flange- defines bone contacting surface (US20060195103)
- Spikes or Tabs- Assist in the wedging of the anchor within the bone (US20060155287)
- Curved legs (US20050273138)
Patent landscape by anchor component
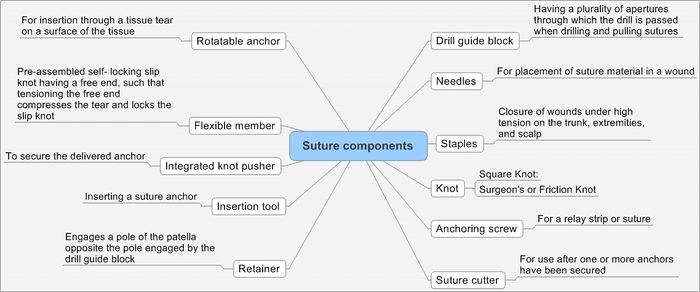
Suture componenets:-
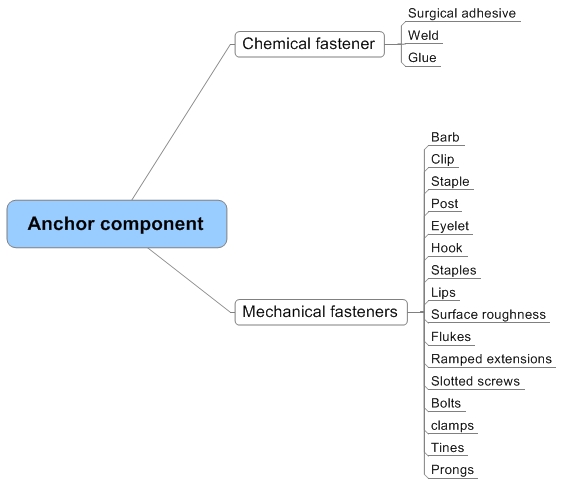
Anchor component
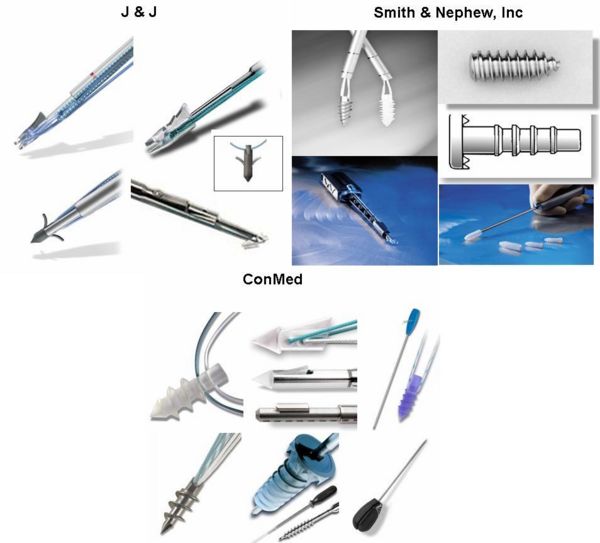
Competitors in these areas
Individual competitors' patents assessed by anchor components
Anchors can be catagorized as:
- Chemical fastener
- Mechanical fastener
| Anchor structure | Chemical fasteners | Mechanical fasteners | Component material | Application | Pat/Publ. No. | Assignee/Inventor |
| Double helix structure | NA | Barb | Biodegradable, biocompatible metals, bioactive substances | Soft tissue or tendon to bone | US20060195103 A1 | Culbert, Brad, S. | von Hoffmann, Gerard | Cachia, Victor, V. |
| Hook-like terminal | NA | Barb, clip, staple, post, eyelet, and hook | Autologous tissue, xenograph material, and synthetic. | prosthetic heart valve | US20060052867 | Medtronic |
| Continuous wire | Surgical adhesive | Barbs, sutures, staples, and combinations, magnetic fastener | Biologically compatible resilient material | Gastrointestinal tract | US20050125020 | GI Dynamics |
| Sleeve-like structure, tubular stent-like structure, helical coil, polymeric tube, conical structure and metallic mesh. | Weld, glue, or adhesive | Hooks, lips, surface roughness | Natural and biologic tissue, collagenous material, shape memory, synthetic, or bioresorbable | Heart (preventing formation of thrombi in the left atrial appendage) | US20050070952 | NMT Medical |
| Double helix structure | NA | Barbs, lips, eye or hook | NA | Soft tissue or tendon to bone | US20050033289 | Culbert, Brad, S. |
| Staple (fluke-bearing anchor ) | Surgical glue | Hook, flukes | Viscoelastic material | Soft tissue or tendon to bone | US20030163160 | Bell, Michael, S G | Lee, James | Lee, Leonard, G |
| Conical, spherical | NA | Ramped extensions or barbs | Medical-grade construction materials | Bones or bone fragments | US20030097132 | Culbert, Brad S. | Hoffmann, Gerard von | Cachia, Victor V. |
| Stacked rods is circular or elliptical | NA | Slotted screws, staples, bolts, hooks or clamps | Biocompatible material | Spinal fixation | US20030083749 | Haines, Timothy |
| Single hook, multiple hooks, stent, helix, loop and disk | Glue | Barbs, hook | Biocompatible material | Heart treatment | US20030078465 | Domingo, Nicanor | Whayne, James G |
| Tubular | NA | Tines, prongs, or barbs | Bioabsorbable materials | Knee joint | US20030040795 | Jacobs, Daniel |
Competitive products